Gut dysbiosis: the hidden root cause of digestive issues and how to restore balance
Introduction
If you've been struggling with bloating, irregular bowel movements, or unexplained fatigue, the answer might lie in your gut microbiome. Gut dysbiosis - an imbalance in the bacteria, fungi, and other microbes living in your digestive system - is increasingly recognised as a root cause of not just digestive issues, but also problems with energy, hormones, skin, and even mental health.
The good news? Once you understand what's happening in your gut, there are clear, evidence-based steps you can take to restore balance.
In this guide, we'll explain what dysbiosis means, how it affects your whole body, and the nutritional strategies that can help you feel better.
In this article:
What is gut dysbiosis?
Put simply, dysbiosis means the balance of microbes in your gut has been disrupted. Your gut microbiome contains trillions of bacteria, fungi, and other microorganisms that play essential roles in digestion, immunity, and overall health. When this ecosystem is in balance, the helpful microbes keep the harmful ones in check.
Gastrointestinal dysbiosis occurs when this balance tips the wrong way - too many harmful microbes, not enough beneficial ones, or a lack of diversity overall.
This imbalance doesn't just affect your digestion. Because your gut microbiome influences everything from nutrient absorption to hormone regulation to brain chemistry, dysbiosis can have far-reaching effects throughout your body.
Common signs and symptoms of gut dysbiosis
Gut dysbiosis can show up in many different ways, and the symptoms aren't always obviously connected to digestion.
Digestive symptoms:
Bloating, especially after meals
Abdominal pain or discomfort
Diarrhoea or constipation (or alternating between both)
Excessive gas
Heartburn or reflux
Wider body symptoms:
When gut health is compromised, you might also experience:
Skin problems such as acne, eczema, or unexplained rashes
Low energy and fatigue that doesn't improve with rest
Weakened immunity with frequent colds or infections
Hormone imbalances affecting your menstrual cycle
Mental health changes including anxiety, low mood, or brain fog
If you're experiencing a combination of these symptoms, particularly digestive issues alongside fatigue or mood changes, an imbalanced gut microbiome could be a contributing factor.
What causes gut dysbiosis
Many factors can disrupt your gut microbiome - and some may have started before you were even born.
Diet-related factors
A diet low in variety and colour (limited plant diversity)
High intake of processed foods and refined sugars
Low fibre intake
Food additives and emulsifiers
Lifestyle and environmental factors
Chronic stress
Antibiotic use (even a single course can disrupt the microbiome for months)
Travel infections or food poisoning
Early life factors
Your gut microbiome begins developing at birth and is shaped by factors like delivery method (vaginal vs caesarean), breastfeeding, early antibiotic exposure, and childhood diet. This means some people may be more susceptible to gut issues from an early age.
The gut-hormone connection for women
For women, the relationship between gut health and hormones is particularly significant. Your gut microbiome directly influences how your body produces, processes, and eliminates hormones.
Oestrogen recycling
Dysbiotic bacteria can recycle oestrogen, affecting the levels of oestrogen. This can contribute to symptoms of hormonal imbalance throughout your menstrual cycle, including PMS (bloating, mood swings, fatigue), painful periods (dysmenorrhoea), and worsening menopause symptoms.
The constipation connection
Sluggish digestion causes hormones like oestrogen to be reabsorbed through the gut wall rather than eliminated. This is one reason why addressing constipation is often a key part of supporting hormonal balance.
Stress hormones and adrenal health
Gut dysbiosis can elevate cortisol, your primary stress hormone. Chronically elevated cortisol impacts your adrenal glands and can contribute to imbalances in sex hormones, as well as symptoms like fatigue and difficulty maintaining a healthy weight.
Blood sugar and insulin
Your gut microbiome influences how your body regulates blood sugar through insulin. Dysbiosis can affect insulin sensitivity, impacting your energy levels, weight, and long-term metabolic health.
Thyroid function
Gut infections resulting from dysbiosis can affect thyroid function. Since the thyroid acts as your body's ‘master hormonal regulator’, this can lead to symptoms including fatigue, low mood, irregular bowels, and poor temperature control.
Get a free 7-day hormone rebalance plan
Download a free guide designed by our nutritionists here and start supporting your hormones through nutrition
The gut-brain connection
You've probably heard of the ‘gut-brain axis’ - but what does this actually mean for your health?
The vagus nerve: your communication highway
Central to the gut-brain connection is the vagus nerve, which carries signals between your brain, heart, and digestive system. This nerve is part of your parasympathetic nervous system - the ‘rest and digest’ mode that allows proper digestion to occur.
When the vagus nerve isn't functioning optimally (due to chronic stress, trauma, or other factors), digestion suffers. This can affect nutrient absorption, bowel regularity, and ultimately contribute to gut dysbiosis.
Bidirectional communication
The communication along the vagus nerve goes both ways. Stress, trauma, or emotional experiences affect your gut microbes. In turn, your gut microbes produce neurotransmitters - brain chemicals like serotonin and dopamine - that influence your mood, anxiety levels, energy, sleep, and appetite.
Your gut makes brain chemicals
In a healthy, balanced gut microbiome, beneficial microbes produce the building blocks for serotonin synthesis in the brain. They also produce short-chain fatty acids (SCFAs) that can cross the blood-brain barrier and help reduce inflammation in the brain. This may help prevent symptoms like low mood, anxiety, and fatigue.
This explains why many people notice improvements in their mental health when they address their gut issues - the connection is very real and very physical.
How dysbiosis is diagnosed
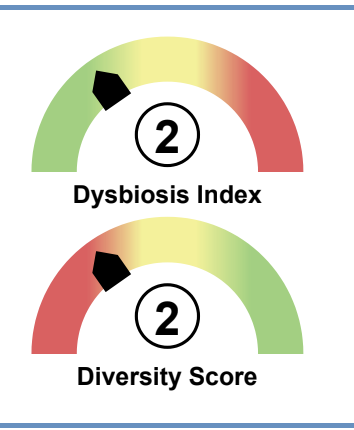
At Peach Health, we use comprehensive functional gut health testing to get a detailed understanding of what's happening in your gut microbiome.
GI360 and similar functional tests
Functional gastrointestinal testing involves collecting stool samples over up to three days. This comprehensive approach analyses your gut microbiome in detail, identifying parasites and pathogens, fungi and yeast strains, beneficial bacteria levels, and your overall ‘dysbiosis index’.
Why interpretation matters
The test results are only as useful as the interpretation. Understanding how your specific results relate to your individual symptoms is key to creating a personalised treatment plan with the best chance of success.
This is where working with a qualified practitioner makes a real difference. At Peach, our nutritionists are trained to interpret these complex reports and translate them into practical, targeted interventions.
Curious about testing?
Our practitioners use comprehensive functional testing including GI360 to create personalised plans for resolving gut issues.
Book a free call to discuss whether testing could be helpful for you
Evidence-based treatment approaches
Here's something that might surprise you: probiotic supplements aren't always the answer - and in some cases, they can actually make things worse.
Why we work from top to bottom
At Peach, we approach dysbiosis treatment by looking at your gastrointestinal system from the top down. This is because the function of your upper gut (mouth, stomach) often needs to be addressed first to create a favourable environment in your lower gut where beneficial microbes can thrive.
If you skip this step and go straight to probiotics, you may be trying to populate a gut that isn't ready to support them.
Supporting the gut lining
The health of your gut wall and its protective mucosa layer is essential for good bacteria to flourish. This lining also protects approximately 70% of your immune system, which sits just behind the gut wall.
Healing and supporting this barrier is often a crucial step before introducing new microbes.
Rebalancing the microbiome
Once the upper gut and gut lining are supported, we can work on the balance of microbes themselves. This may involve prebiotics (fibres that feed beneficial bacteria), specific probiotic foods or supplements chosen for your individual needs, and gentle antimicrobials to target specific pathogens or parasites identified through testing.
The key is personalisation - what works for one person may not work for another, which is why comprehensive testing and expert interpretation are so valuable.
Dietary strategies for restoring gut balance
Food is medicine when it comes to gut health. Here are the dietary strategies we use at Peach to support gut healing.
Supporting upper gut function
Mindful eating habits: Slowing down, chewing thoroughly, and eating in a relaxed state
Bitter foods: Rocket, radicchio, and other bitter leaves stimulate digestive secretions
Ginger: Supports stomach motility and digestive comfort
Beetroot: Supports bile flow and liver function
Supporting the gut lining
Foods to reduce or remove:
Processed foods containing emulsifiers
Refined grains
Foods you've identified as personal triggers
Foods to include:
Organic or homemade bone broths (rich in gut-healing compounds)
Stewed apples (contain pectin that supports the mucosa)
Anti-inflammatory foods like certain seeds and oily fish
Building a healthy microbiome
Once your gut is ready, a slow, gradual introduction of:
Prebiotic foods: A variety of colourful vegetables, herbs, spices, and legumes
Probiotic foods: Kefir, sauerkraut, and kimchi (depending on individual tolerance)
The emphasis on slow and gradual is important. Increasing fibre too quickly can worsen symptoms in some people, so pacing is key.
Dysbiosis vs SIBO vs other gut conditions
Understanding the differences between various gut conditions can help you communicate with healthcare providers and understand your diagnosis.
Dysbiosis
Describes the overall imbalance in gut microbes. It's a broad term that can apply to various types of microbial disruption.
SIBO (Small Intestinal Bacterial Overgrowth)
SIBO occurs when bacteria that normally live in the large intestine (colon) migrate into the small intestine, where they don't belong. This causes fermentation of food in the wrong place, leading to bloating, pain, and other symptoms. SIBO is a specific type of dysbiosis.
IBS (Irritable Bowel Syndrome)
IBS is a diagnosis based on symptoms of gut dysfunction - pain, bloating, altered bowel habits - without visible inflammation. Dysbiosis and SIBO are common underlying factors in IBS.
IBD (Inflammatory Bowel Disease)
Unlike IBS, IBD involves actual inflammation in the gut and includes conditions like Ulcerative Colitis, Crohn's Disease, gastroenteritis, gastritis, and diverticulitis. These conditions require medical management alongside nutritional support.
Other inflammatory conditions
Inflammation can also occur in the oesophagus (often from long-term acid reflux) or pancreas (pancreatitis). These are distinct conditions that may coexist with or contribute to dysbiosis.
When to seek professional help
If you're experiencing any of the following, it's worth consulting a healthcare professional:
Constipation: Fewer than one to two bowel movements daily
Diarrhoea: Loose or urgent stools regularly
Sporadic pain: Abdominal discomfort that comes and goes
Frequent bloating: Especially if it affects your quality of life
Reflux or heartburn: Particularly if it's persistent
The encouraging news is that many gut issues can be resolved through everyday, small, habitual lifestyle and dietary shifts. You don't always need dramatic interventions - often, it's about working with your body's natural healing capacity.
However, getting the right guidance from the start can save you months of trial and error and help you avoid approaches that might make things worse.
Frequently asked questions
-
Dysbiosis means the balance of helpful bacteria, fungi, and other microbes in your gut has been disrupted - typically with too many harmful microbes and not enough beneficial ones. This imbalance can affect digestion, immunity, hormones, and even mental health.
-
Yes. Your gut microbiome produces neurotransmitters and other compounds that affect brain function. When the gut is out of balance, this can contribute to fatigue, difficulty concentrating, and brain fog. The gut-brain connection is bidirectional, meaning gut health directly influences how you feel mentally and physically.
-
This varies significantly depending on the severity of the imbalance, underlying causes, and how consistently you follow a treatment plan. Some people notice improvements within weeks, while others may need several months of targeted support. Working with a practitioner who can personalise your approach typically leads to faster, more sustainable results.
-
Not necessarily. In some cases, taking probiotics before addressing other issues (like stomach acid levels, gut lining health, or existing infections) can actually worsen symptoms. This is why a systematic approach - working from the top of the digestive system down - is often more effective than jumping straight to probiotic supplements.
-
Dysbiosis is a general term for microbial imbalance in the gut. SIBO (Small Intestinal Bacterial Overgrowth) is a specific type of dysbiosis where bacteria that normally live in the large intestine have migrated into the small intestine. Both can cause similar symptoms like bloating and digestive discomfort.
Key takeaways
Gut dysbiosis is an imbalance in your gut microbiome that can cause digestive issues and affect your whole body, including energy, hormones, skin, and mental health
Many factors contribute to dysbiosis, including diet, stress, antibiotics, and even factors from early life
For women, gut health is closely connected to hormone balance, affecting everything from your menstrual cycle to menopause symptoms
The gut-brain connection means improving gut health can positively impact mood, anxiety, and cognitive function
Comprehensive gut health testing like GI360 provides detailed insights that guide personalised treatment
Effective dysbiosis treatment works from the top of the digestive system down, addressing stomach function and gut lining before rebalancing microbes
Dietary strategies including bitter foods, gut-healing foods like bone broth, and gradual introduction of prebiotics and probiotics can support recovery
Ready to get support?
If you're tired of struggling with digestive issues, unexplained fatigue, or symptoms that seem disconnected but might all trace back to your gut, our team at Peach Health can help. We offer personalised nutrition strategies including comprehensive gut health testing to understand what's really going on and create a tailored plan to restore balance.
Book a free discovery call to learn how we can support you, or explore our gut health services to find out more about our approach.